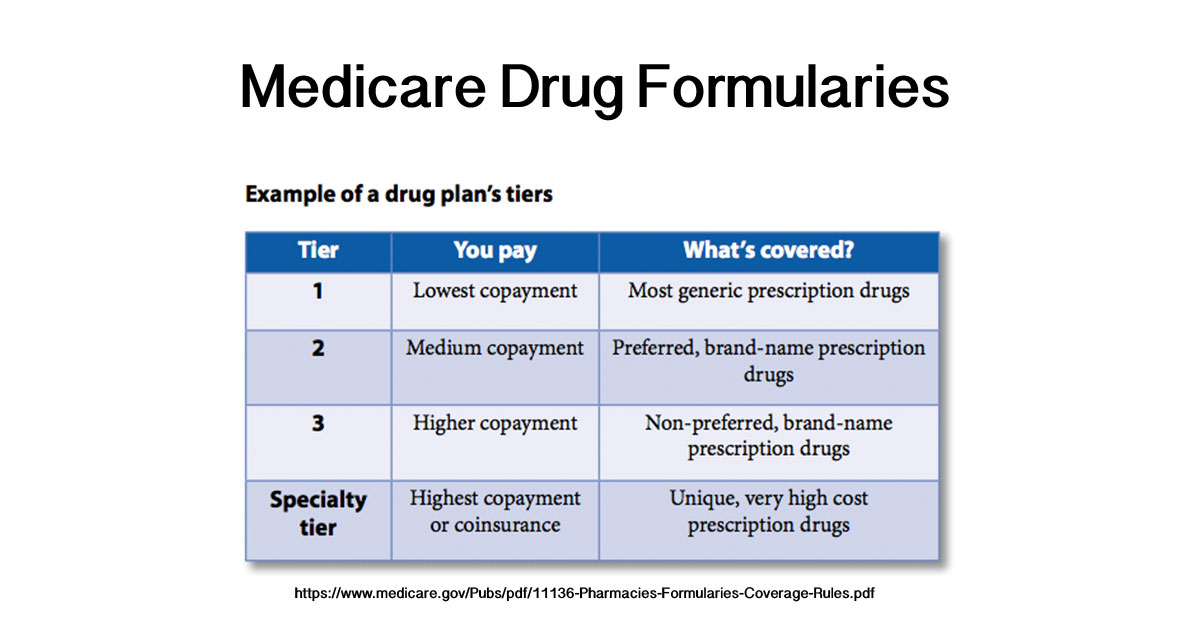
Covered prescription drugs are assigned to 1 of 4 different levels with corresponding copayment or coinsurance amounts. 105 - Medical Supplies Associated with the Delivery of Insulin.
 See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Illinois
See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Illinois
This list shows prescription drug products in tiers.

Tier 6 drugs. After your first 30-day supply we will not pay for these drugs even if you have. For each of your drugs that is not on our formulary or if your ability to get your drugs is limited we will cover a temporary 30-day supply unless you have a prescription written for fewer days when you go to a network pharmacy. For most plans youll pay 0-5 for drugs in this tier.
This list shows prescription drug products in tiers. This is also kinda one of those drugs ive done videos as well I suppose. Most Medicare plans have a 4 or 5 tier formulary.
Level or Tier 1. The levels are organized as. 104 - Extemporaneous Compounds.
Only use the search function below to identify if a prescription is an approved drug in a 6-tier benefit plan. Many common brand name drugs called preferred brands and some higher-cost generic drugs. Drugs Moving from Tier 5 to Tier 6 ACTEMRA INJ 162 MG09 ML ELIGARD INJ 30 MG ADCIRCA TAB 20 MG ELIGARD INJ 45 MG.
Generally each drug is placed into one of up to six member payment tiers. Tier 4 Non-preferred brand name drugs - 35 of retail cost-sharing. Brand-name drugs are capitalized eg AMOXIL and generic drugs are listed in lower-case italics eg amoxicillin.
The Drug Formulary is subject to change without. Please refer to your Certificate of Coverage Master Contract Plan Document or other plan materials to determine if your drug is covered. Generic drugs which could be low-cost preferred generics or general preferred generics.
Level or Tier 3. Transmittals for Chapter 6 10 - Definition of a Part D Drug. The prescription drug tier which consists of the higher-cost prescription drugs most are brand-name prescription drugs and some specialty drugs.
Drug Formulary Search. 102 - Covered Part D Drug. Non-preferred generic and non-preferred brand name drugs.
These drugs offer a medium co-payment and are often brand name drugs that are usually more affordable. Brand-name drugs including preferred and nonpreferred options. Generally each drug is placed into one of up to six member payment tiers.
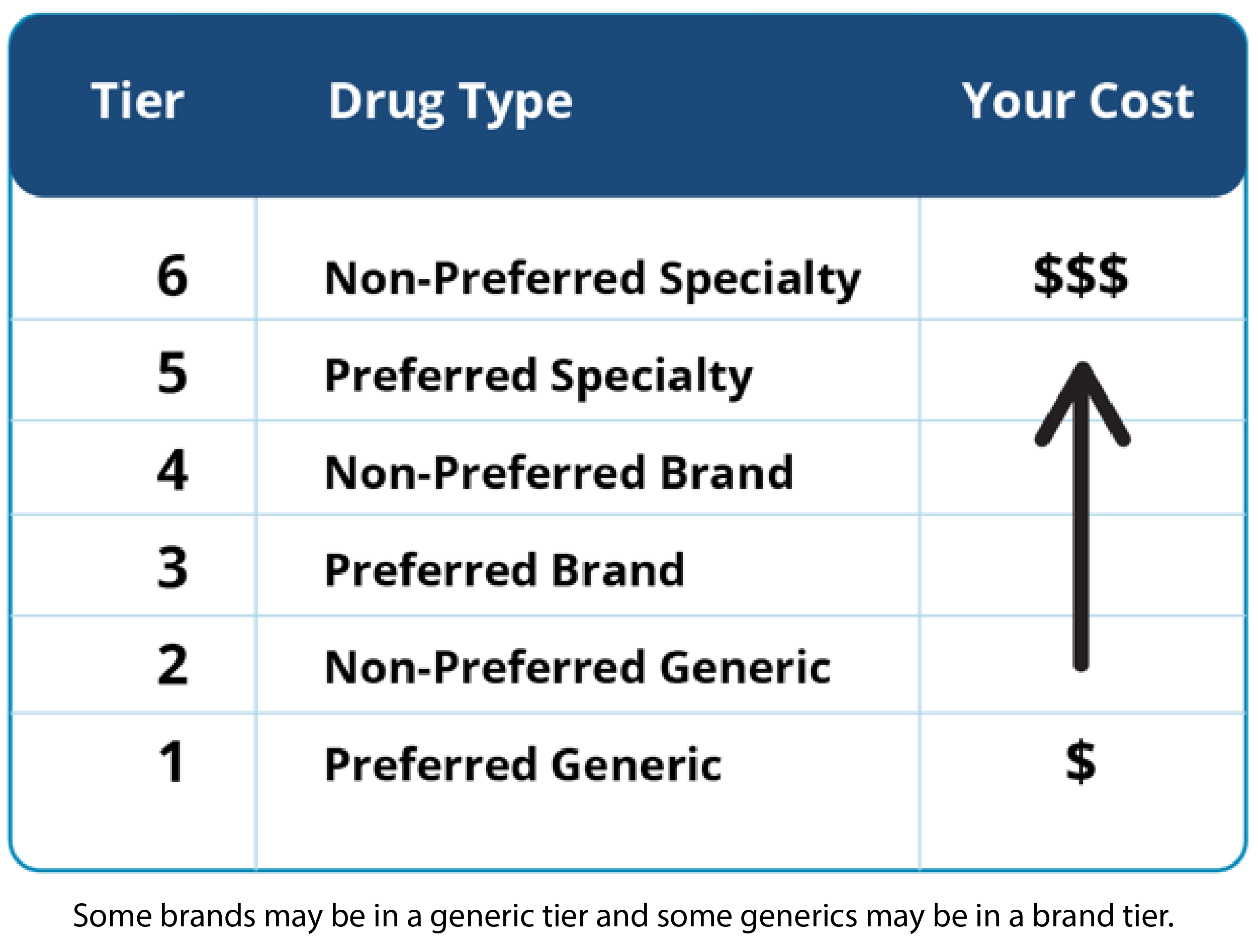
Tier 2 Generic drugs - 10 co-pay. Preferred Generic Tier 1 Non-Preferred Generic Tier 2 Preferred Brand Tier 3 Non-Preferred Brand Tier 4 Preferred Specialty Tier 5. The prescription drug tier which consists of high-cost prescription drugs most are brand-name prescription drugs.
For most plans youll pay 25 to 33 of the retail cost for drugs in this tier. There is not any one correct tier structure for a formulary. 6-Tier Drug Formulary Search With this search tool you can identify whether or not a specific drug will be covered by a plan with 6-tier coverage.
Tier 1 Preferred generic drugs - 0 co-pay. Lower-cost commonly used generic drugs. These drugs offer the lowest co-payment and are often generic version of brand name drugs.
Generally each drug is placed into one of six member payment tiers. These are generic drugs used to treat diabetes and high cholesterol. As an example a plan may form drug tiers this way.
These are the most expensive drugs on the drug list. These drugs have the highest co-payment and are often brand-name drugs that have a generic version available. Generally each drug is placed into one of six member payment tiers.
Some brands may be placed in generic tiers and some generics may be placed in brand tiers. They can be generic or brand name. Preferred Generic Tier 1 Non-Preferred Generic Tier 2 Preferred Brand Tier 3 Non-Preferred Brand Tier 4 Preferred Specialty Tier 5 and Non-Preferred Specialty Tier 6.
Subscribe httpsgooglk3Ga7s SUPPORT. Preferred Generic Tier 1 Non-Preferred Generic Tier 2 Preferred Brand Tier 3 Non-Preferred Brand Tier 4 Preferred Specialty Tier. The prescription drug tier which consists of the highest-cost prescription drugs.
Tier 1 Preferred Generic drugs Tier 2 Non-Preferred Generic drugs Tier 3 Preferred brand name drugs Tier 4 Non-preferred brand name drugs Tier 5 Preferred Specialty drugs Tier 6 Non Preferred Specialty drugs Specialty drugs filled by a specialty pharmacy and limited to a 30-day supply are prescription medications that often require special storage handling and close. Level or Tier 2. Tier 3 Preferred brand-name drugs - 25 of retail cost-sharing.
103 - Commercially Available Combination Products. Drugs Changing from Tier 5 to Tier 6 A Division of Health Care Service Corporation a Mutual Legal Reserve Company an Independent Licensee of the Blue Cross and Blue Shield Association 6139-TX 10-17 1. Preferred Generic Tier 1 Non-Preferred Generic Tier 2 Preferred Brand Tier 3 Non-Preferred Brand Tier 4 Preferred Specialty Tier 5 and Non-Preferred Specialty Tier 6.
Tier list video for all the drugs ive done. 2021 6-Tier Drug Formulary PLEASE READ. The prescription drug tier which consists of some of the highest-cost prescription drugs most are specialty drugs.
The Drug Formulary does not guarantee coverage and is subject to change. Specialty drugs are used to treat complex conditions like cancer and multiple sclerosis. This drug list was last updated on 05012021.
The information in the RequirementsLimits column tells you if our plans have any special requirements for coverage of your drug. THIS DOCUMENT HAS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN. May cover your drug in certain cases during the first 90 days you are a member of our plan.
106 - Medically-Accepted Indication. 1061 - Retrospective Determination of a Medically-Accepted Indication.