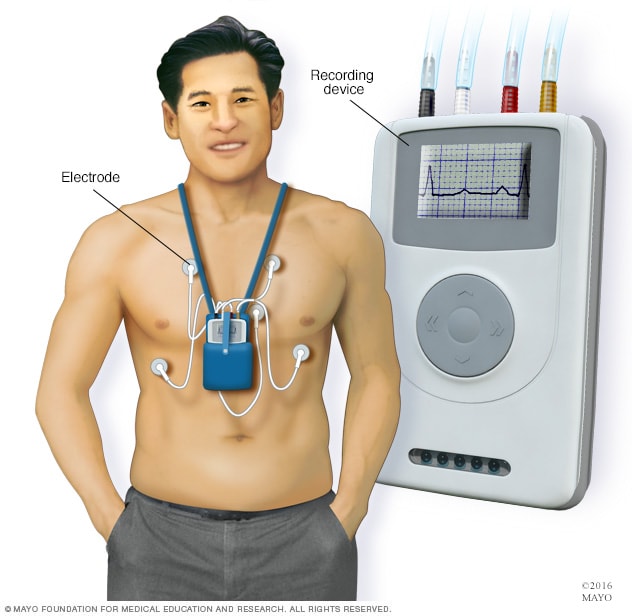
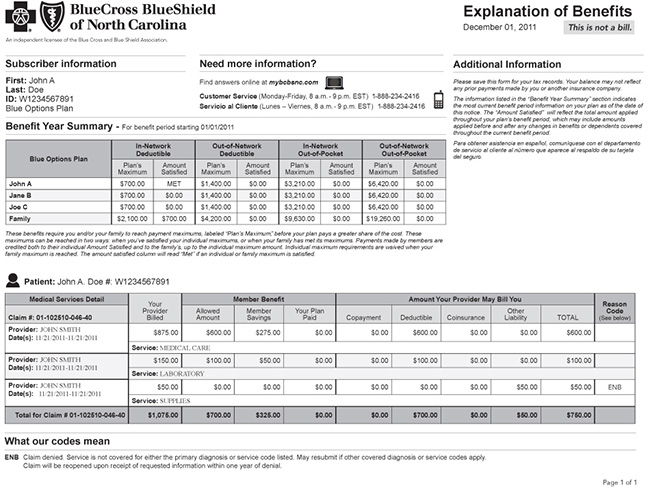
Newer patch -type devices record for longer periods of time. There are two main types of event monitors.
 Holter Monitor Mayo Clinic
Holter Monitor Mayo Clinic
It is activated by the patient when he or she is experiencing symptoms such as dizziness palpitations shortness of breath fainting spells or chest pain to help diagnosis what is causing the symptoms.

30 day event monitor. For self-sensing automatically triggered monitors an EKG is automatically recorded. What is a 30 day event monitoring. Event Monitor including External Loop Recorder.
Recording can be patient-activated when symptoms occur or automatically triggered based on a. Detection of paroxysmal atrial fibrillation by 30-day event monitoring in cryptogenic ischemic stroke. Average of 114 86 days after initiation of monitoring with a median of 2 interquartile range 13 events detected per patient.
Why do people need to use a cardiac event recorder. You can carry or wear a cardiac event monitor up to 30 days. Holter Monitor.
When you activate a symptom event monitor. Most PAF events were asymp-tomatic. Symptom event monitors and memory looping monitors.
The Holter monitor is a portable device that records a single days electrical activity of the central nervous system while the 30 day heart event monitor observes the functioning of the heart over a month. But it does it for longer periods of time usually at least 1 minute. For instance heartbeats that are.
The cardiac event monitor is mainly used to observe or detect any abnormal rhythms of the heart. Event monitors can be worn for weeks or until symptoms occur. The indications of use for Holter Monitoring and Cardiac Event Monitoring is generally straight forward but they can vary slightly from one insurance carrier to the next.
These symptoms may include palpitations also described by patients as irregular beats skipped beats hard beats fluttering rapid beats or pounding. While the cardiac monitor is attached you will go about your regular activities and return the device to your doctor or the cardiac monitoring lab at the end of the procedure. 24 Hr-30 Day Monitoring.
Portable device that records heart rhythms continuousyl for up to 72 hours. Monitoring receipt of transmissions and analysis. Your doctor may recommend an event monitor when symptoms are infrequent less than daily.
Recording can be patient -activated when symptoms occur or automatically. Only 6 of 98 PAF events 61 were from a patient-triggered recording or were associated with patient-. 30 day event monitor.
These connect by wires to the monitor device. There are several types of cardiac event monitors. Cardiac Event Monitors can be worn for a period of up to 30 days if the laboratory has not received any relevant or abnormal transmissions from the Cardiac Event Monitor.
You wear the device for 30 days. QuestIon in 30 day event monitor. Portable device that records and stores heart rhythms continuously for 14-30 days or longer.
Cardiac event monitor technology varies among different devices. An event monitor uses small sticky pads electrodes stuck to your chest. Event Monitor including external loop recorder.
Spade22 Jan 16 2012. While wear the device you proceed with your normal daily activities. A 30-day ambulatory cardiac event monitor Patients will be fitted with dry electrode belt including cardiac event monitorand instructed to wear the device for as many hourswaking and sleeping each day as possible for a total of 30 days.
If your medicines are working. Why Is a Cardiac Event Monitor Used For. Routine monitoring in this population should be strongly considered.
An event monitor is a portable device used to record your hearts electrical activity when you have symptoms. The device records the same kind of information as an electrocardiogram ECG. Portable device that records and stores heart rhythms contni uously for 14 -30 days or longer.
Wearable patient activated electrocardiographic rhythm derived event recording with presymptom memory loop 24-hour attended monitoring per 30 day period of time. A 30 day event monitor is a portable device that you wear that records your hearts electrical activity. Wearing the monitor may tell your doctor.
Cardiac event monitoring is used to record a patients heart rhythm when he or she is experiencing symptoms. Holter vs Event Monitor. Twenty-four percent of events were detected late in the 30-day window Figure.
Hi I am current wearing a 30 day event monitor to try and capture some irregular heart rhythms I feel once in a while. Watch an animation of an arrhythmia. An event monitor is for long-term monitoring up to 30 days.
You may be asked to wear a cardiac event recorder if you have fast slow or irregular heartbeats called arrhythmias. Most of these devices can transmit the recorded information directly to your healthcare provider. This allows him or her to analyze the electrical activity of your heart while.
The data taken from the monitor about when arrhythmias occur and where in the heart they are coming from can help your. For patient-activated event monitors the patient initiates recording when symptoms appear or when instructed to do so by a physician eg following exercise. Your doctor may order 24 hour30 day cardiac event monitoring for you to help evaluate any of a variety of symptoms to determine if these symptoms are related to your heart.
The Stroke and Monitoring for PAF in Real Time SMART Registry -Approximately 1 in every 9 patients with cryptogenic ischemic stroke was found to have new PAF within 30 days. Today I felt several minutes of continuous. The event monitor captures events and records them on its own and I can also push the record button if I feel something.
You carry the device in your hand wear on your wrist or keep it in your pocket. Patient typically wears the device for 20 or 30 days. It records the same information as an electrocardiogram ECG but for longer durations of time.
Applied Cardiac Systems ACS CardioNet.
Https Ahmspro Com W Logins Www Silverscript Com Login Php