Recently Humana added many benefits to its Medicare Advantage plans. In fact 88 of Medicare Advantage plans cover hearing aids in 2021.
 Medicare And Hearing Aids Coverage Exclusions And More
Medicare And Hearing Aids Coverage Exclusions And More
The majority of major insurers who offer Medicare Advantage plans have at least one plan that covers hearing aids.

Medicare plans that cover hearing aids. Medicare Supplement Plans. HMOs usually include coverage for prescription drugs as well as other optional benefits such as routine hearing services. Annons Vi hjälper dig att hitta rätt hörapparat som passar just dina behov.
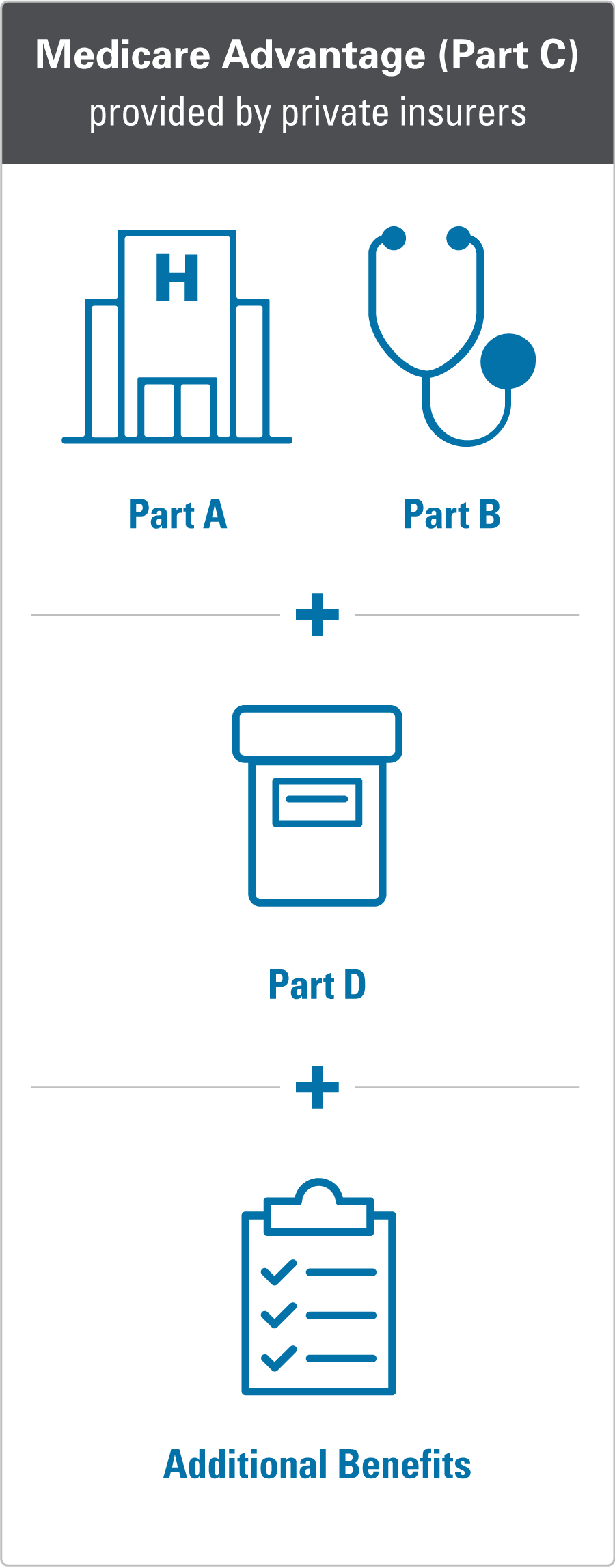
Annons Professionell fotvårdserie framtagen av ledande specialister inom medicinsk fotvård. Some Medicare Advantage Plans Part C offer extra benefits that Original Medicare doesnt cover - like vision hearing or dental. Annons Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more.
Annons Improve Your Business ROI - Get A Better Deal On Aids Hearing. Medicare Advantage plans can add the following hearing insurance for seniors benefits. Original Medicare the name for Medicare Part A and Part B does not pay for hearing aids typically but it may cover hearing exams.
Vi erbjuder ett brett sortiment av hörapparater anpassade för dina behov. One of these benefits is hearing benefits including the cost of hearing aids. Without insurance to cover or supplement the costs of hearing aids your cost per hearing aid could be in the range of 2400 each.
Health Maintenance Organizations HMOs. Handla enkelt fraktfritt med snabb leverans. These insurers include Humana Aetna and Blue Cross Blue Shield.
Annons Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more. However some seniors may not be eligible for those plans and the plans may have a higher premium than those that dont offer hearing aid coverage. Some of the best plans available to cover hearing aid costs are through Humana.
Although Original Medicare benefits do not cover hearing tests or hearing aids it is possible that you could receive either full coverage partial coverage or a reimbursement for expenses related to hearing aids through a supplemental insurance plan. Lykos hår- Skönhetsvärld. This is because Medicare Supplement or Medigap policies may provide benefits through various partnerships with.
Find affordable quality Medicare insurance plans that meet your needs. However some Medicare Part C plans may include coverage for hearing services including hearing aids. The next question might be whether or not a Medicare supplement policy Medigap would cover any of your hearing aid expenses.
Find affordable quality Medicare insurance plans that meet your needs. Medicare consists of different parts. Some Medicare Advantage plans Medicare Part C may cover hearing aids however.
Original Medicare parts A and B doesnt cover hearing aids. Dont Buy Meticore Unless Youve Seen This Massive Discount Exclusive Bonuses. Boka en tid här.
Medicare Advantage Plans that Cover Hearing Aids The easiest way to get Medicare coverage for audiology appointments treatments hearing aids is to enroll in a Medicare Advantage plan. Treatments for hearing problems Hearing aids Hearing aid fittings Hearing aid. At this time none of the 10 Medicare supplement plans.
Depending on where you live you may be eligible for one of these two types of Medicare Advantage plans that may include coverage for hearing aids. Vi erbjuder ett brett sortiment av hörapparater anpassade för dina behov. Boka en tid här.
While some separate hearing benefit plans are available its often not as cost-effective. Annons Vi hjälper dig att hitta rätt hörapparat som passar just dina behov. Contact the plan for more information.
Annons You must order now to get Meticore and secure your order while stocks last.











.png)