Drug Recall List PDF Using your drug list. Tier 3 preferred brand.
 Medicare Drug List Drug Plans Options And Costs
Medicare Drug List Drug Plans Options And Costs
New products in a reviewed drug class.

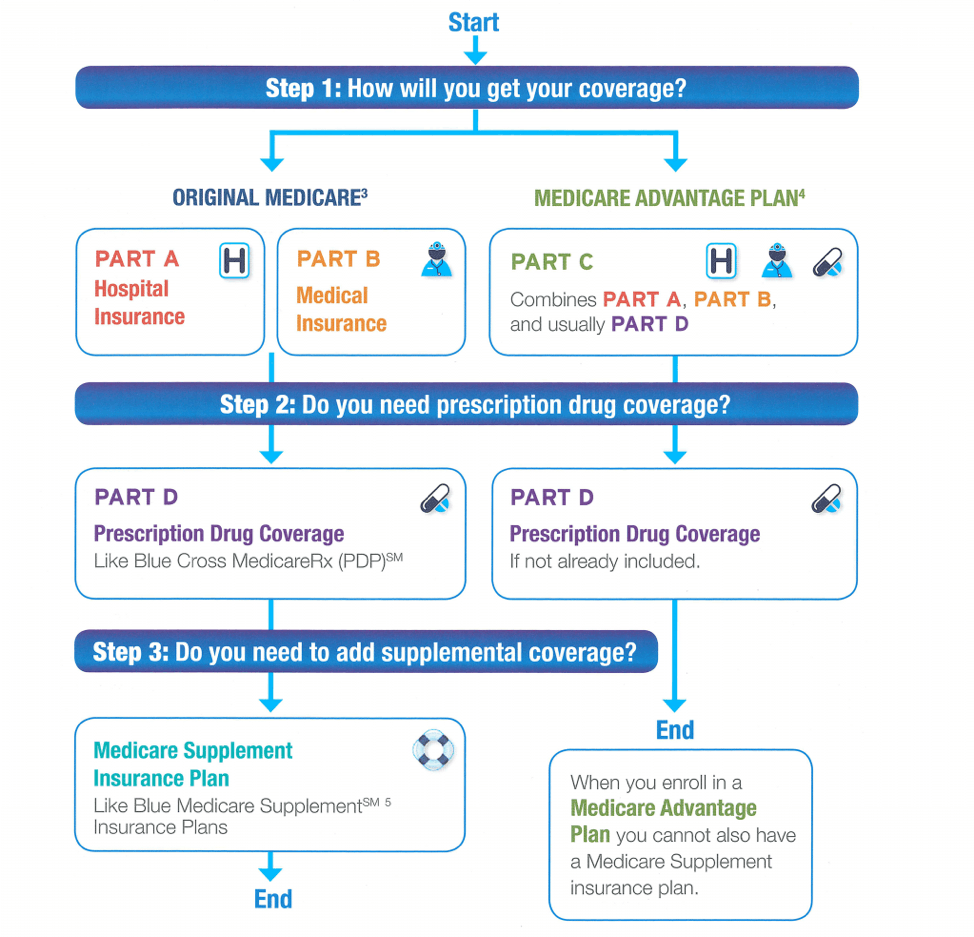
Preferred drug list for medicare. Check our drug list. The Medicare Part D Formulary is a list of covered drugs on your prescription drug plan. Complete Blue PPO Distinct.
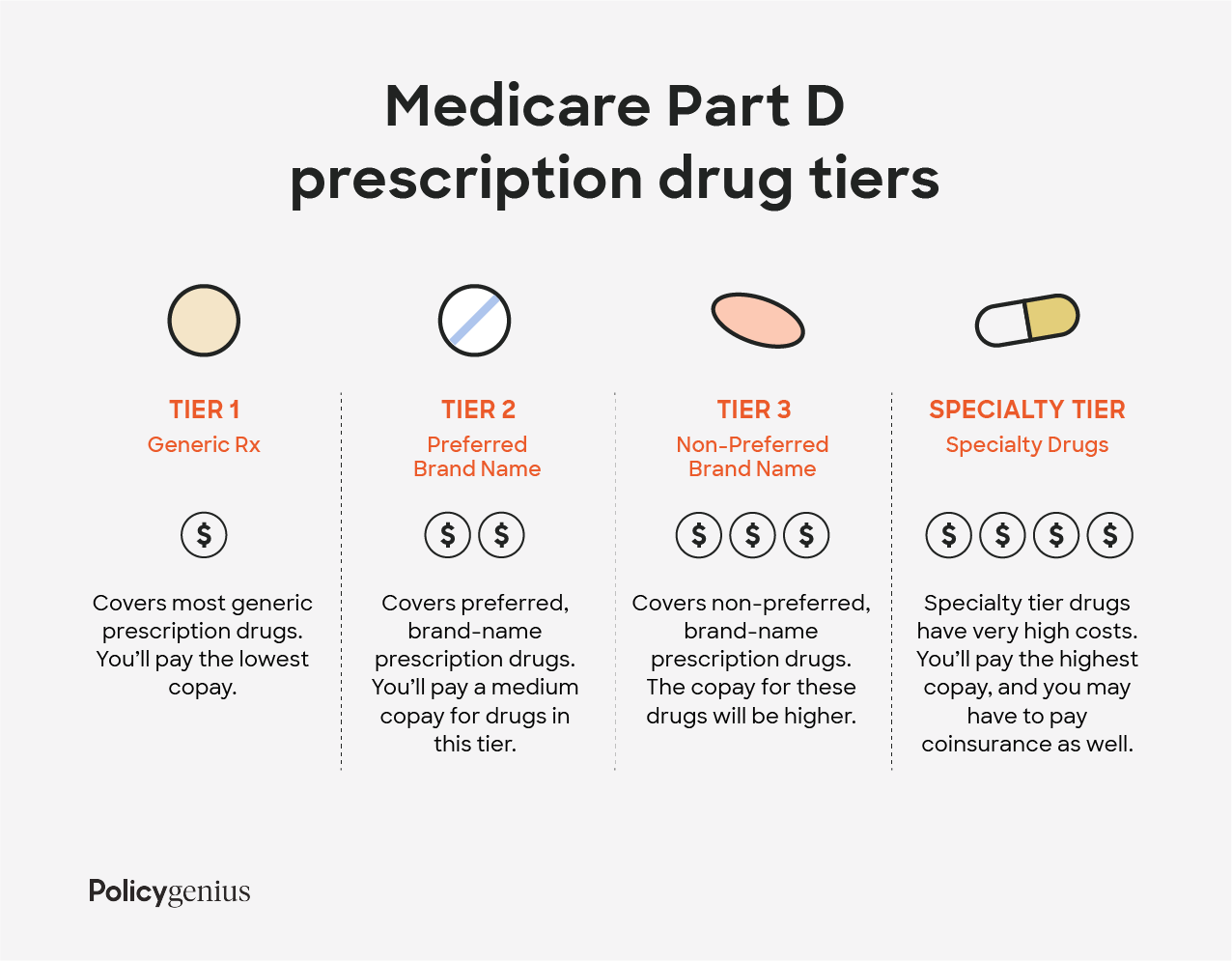
Tier 4 non-preferred drugs. THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN HPMS Approved Formulary File Submission ID 00020556 Version Number 26 Y0011_34655_C 0818 C. Youll want to find the formulary that fits with the medications you take.
Medicare covers flu shots pneumococcal shots Hepatitis B shots and some other vaccines when theyre related directly to the treatment of an injury or illness. These prescription drugs are lower in cost than tier 5. But it can be hard to predict next years prescriptions.
If you have a prescription for a recalled drug talk to your pharmacist about a replacement. Non-preferred generic and non-preferred brand name. Preferred generic Tier 2.
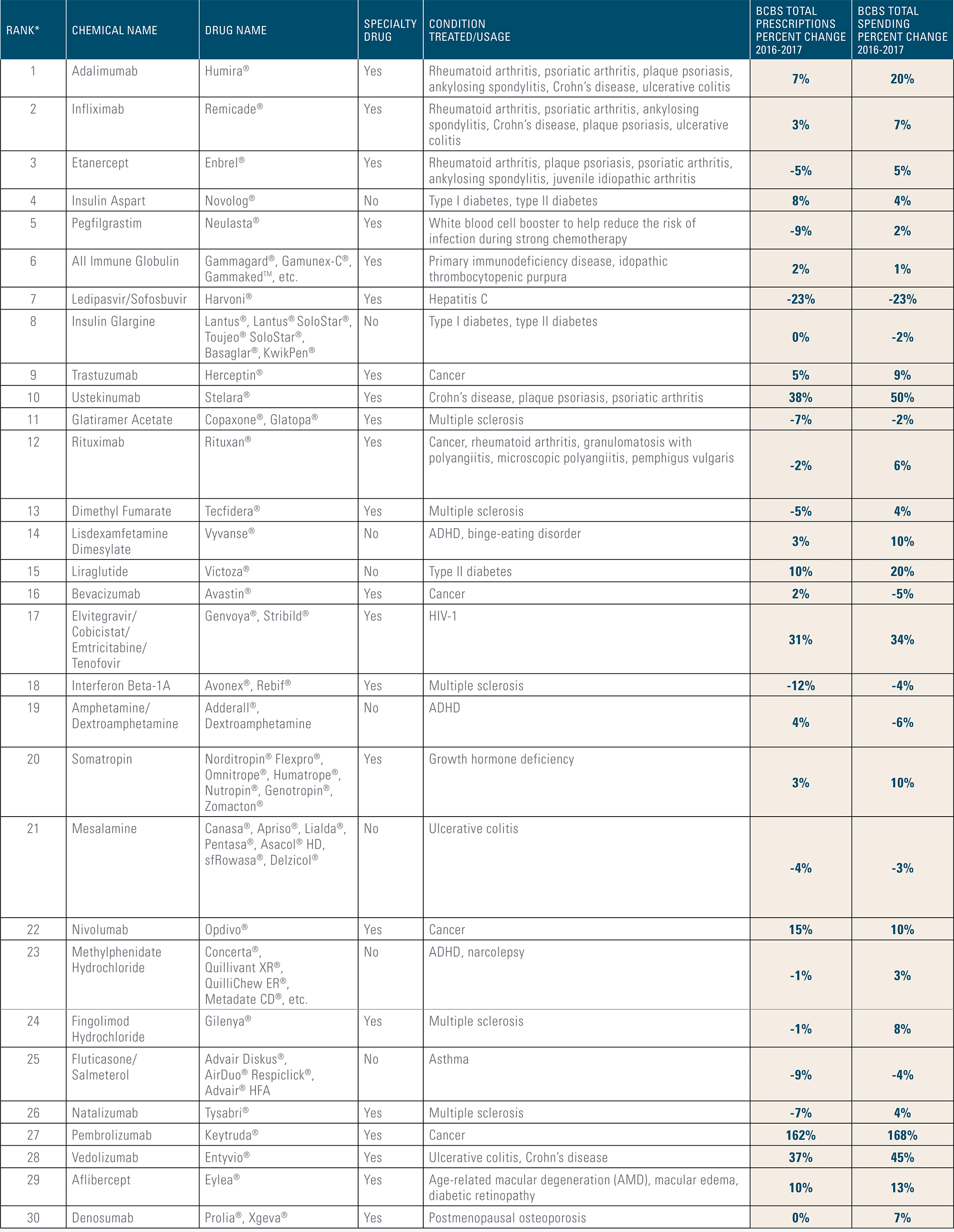
Antidepressants anti-convulsants anti-psychotics immunosuppressants cancer drugs and HIVAIDS drugs. This document has information about the drugs covered by this plan. Medicare also requires Part D prescription drug plans to cover almost all drugs in these six classes.
These are the highest cost drugs including some injectables. Community Blue Medicare Plus PPO Distinct. Select Insulin Drugs Select Insulin Drugs with 35 max copay through gap.
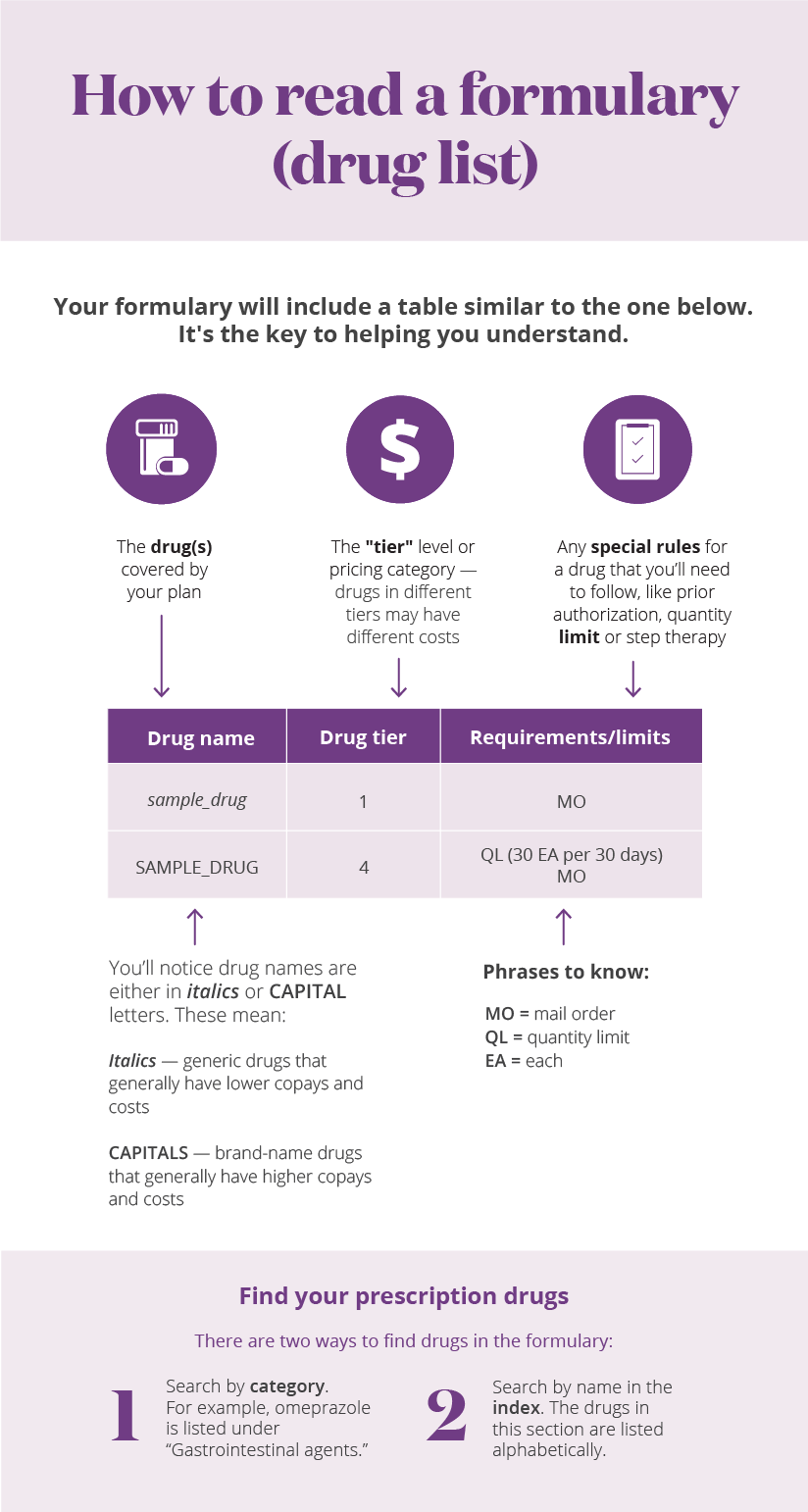
A Prescription Drug List PDL also called a formulary is a list of commonly used medications organized into cost levels called tiers. Minnesota Senior Health Options MSHO has one tier but your copay depends on whether its a generic or a brand-name drug. Tier 2 generic.
If you have Group Medicare through your employer please refer to the Prescription Drug Guide PDG section of your Evidence of Coverage EOC document to find your plan type. Tier 5 specialty. Transplant immunosuppressive drugs.
Freedom Blue PPO Distinct WV Freedom Blue PPO Standard WV Freedom Blue PPO ValueRx. Toll Free 1-800-424-7895 and choose the PDL option. These prescription drugs are lower in cost than tier 4.
Community Blue Medicare HMO Signature. Medicare HMO C-SNP Allwell Medicare HMO Allwell Medicare PPO Allwell Medicare Boost HMO Allwell Medicare Boost P3 HMO Allwell Medicare Boost USHS HMO Allwell Medicare Essentials HMO Allwell Medicare Premier HMO. COMPLETE DRUG LIST FORMULARY Prescription drug list information AARP Medicare Advantage HMO AARP Medicare Advantage HMO-POS AARP Medicare Advantage Plan 1 HMO AARP Medicare Advantage Plan 2 HMO AARP Medicare Advantage Plan 3 HMO Important Notes.
Generally the lower the tier the less you pay. Preferred Drug List Prescribers may request an override for non-preferred drugs by calling the Magellan Medicaid Administration MMA Help Desk at. Choose your plan below to download your drug.
Security Blue HMO-POS ValueRx. However Medicare Part A covers methadone when used to treat an opioid use disorder as an inpatient in a hospital and Part B now covers methadone when you receive it through an. To see a list of commonly covered drugs the formulary simply select your plan year and plan name below.
Many common brand name drugs called preferred Preferred brand brands and some higher-cost generic drugs. Check your PDL to stay updated on your pharmacy coverage. It shows the drugs we cover the tier a drug is on any limits or requirements and mail order availability.
PRESCRIPTION DRUG LIST OF COVERED DRUGS PLEASE READ. Community Blue Medicare PPO Signature. Search our formulary for covered drugs and get the information you need.
The Department of Human Services the department maintains a Statewide Preferred Drug List PDL to ensure that Medical Assistance MA program beneficiaries in the Fee-for-Service FFS and HealthChoicesCommunity HealthChoices Managed Care Organization delivery systems have access to clinically effective pharmaceutical care with an emphasis on quality safety and. It also covers drugs like methadone and buprenorphine when prescribed for pain. Contact your doctor if youve taken a recalled drug and youre feeling ill.
Preferred brand drugs and select insulin drugs. Doctor and outpatient health care or Medicare Part D prescription drugs depending on how it is used. Select from the options below to download and print.
Lower-cost commonly used generic drugs. Medicare drug coverage includes drugs for medication-assisted treatment for opioid use disorders. These prescription drugs usually have a higher cost share than tier 1 drugs.
082019 FHCP Medicare Rx Plus HMO-POS FHCP Medicare Rx HMO FHCP Medicare Rx Savings HMO FHCP Medicare. The plan can change the formulary anytime but they must notify you. Each plan has a different list of drugs.
These costs are decided by your employer or health plan. Your Summary of Benefits tells you the drug costs for tiers. You can print out the full list of drugs covered by Humana called the Prescription Drug Guide.
Youll need to know your pharmacy plan name to complete your search. Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Non-preferred drug Non-preferred generic and non-preferred brand name drugs.
Your pharmacy plan covers thousands of drugs. If you dont get prior approval. This Preferred Drug List is subject to change without notice.
Drugs are recalled either by the drugs maker or the FDA when theyre deemed unsafe. Complete Drug List Formulary 2021 UnitedHealthcare Group Medicare Advantage.