Eligible commercially insuredcovered patients with no restrictions step-edit prior authorization or NDC block and with a valid prescription for TRELEGY ELLIPTA fluticasone furoate umeclidinium and vilanterol inhalation powder who present this savings card at participating pharmacies will pay as little as 0 for each covered 30- 60- or 90-day supply 13 inhalers of TRELEGY. Where can I get more information.
 Trelegy Ellipta Reduces Copd Exacerbations And Improves Lung Function
Trelegy Ellipta Reduces Copd Exacerbations And Improves Lung Function
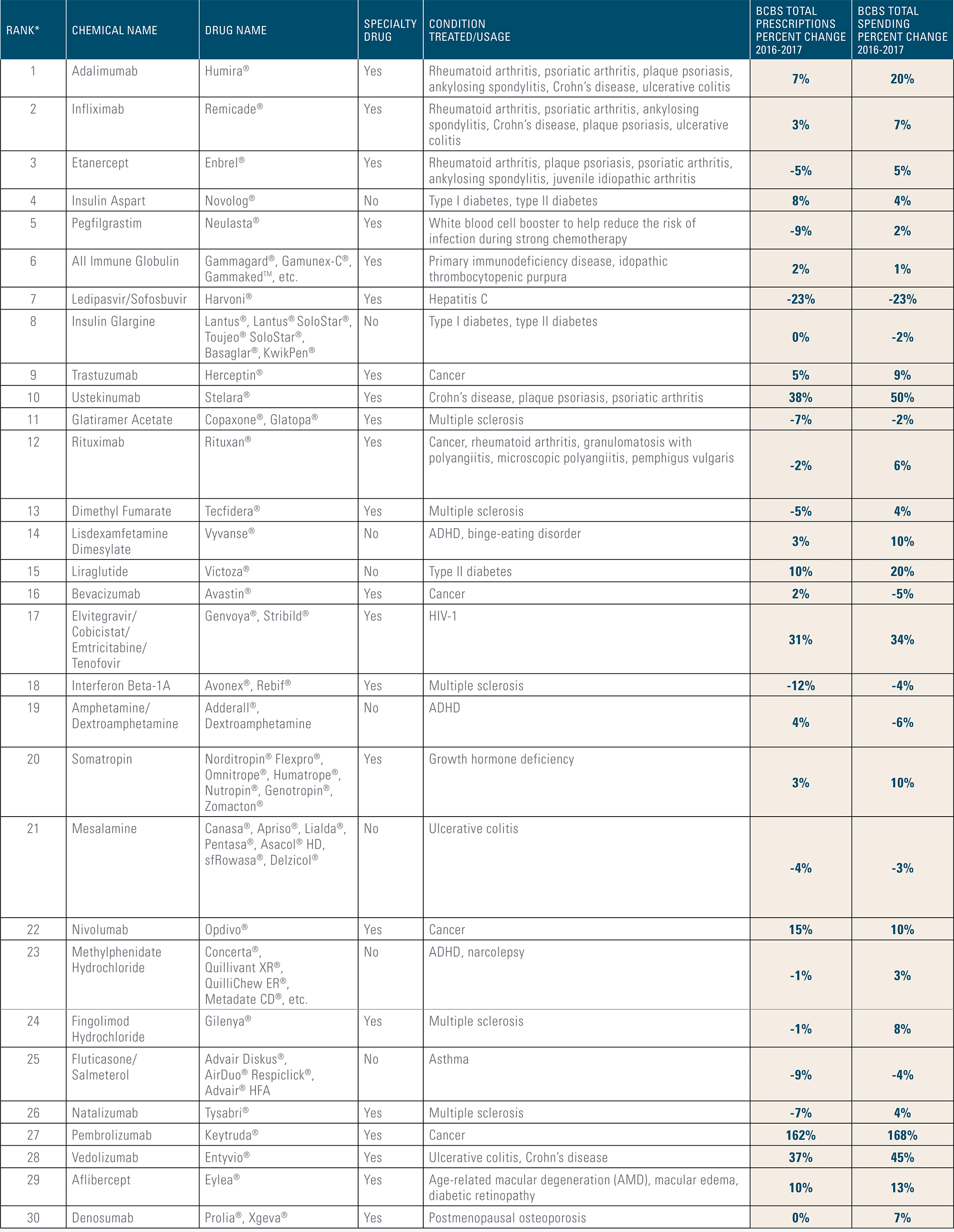
Consult your healthcare provider about the best options for purchasing your medications.

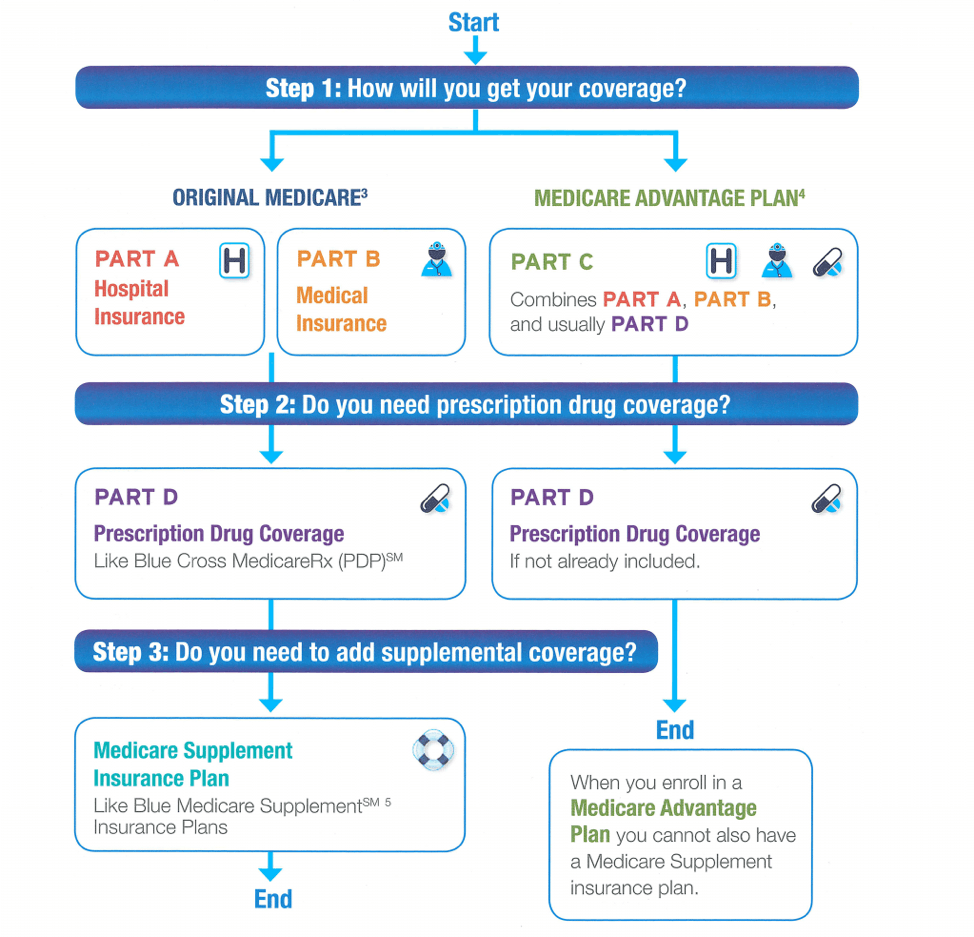
Is trelegy ellipta covered by medicare. Below is the formulary or list of prescription drugs available to enrollees for every 2019 Medicare Advantage Plan in Indiana and 2019 Medicare Part-D in Indiana plans that offers additions coverage for Trelegy Ellipta 100. Trelegy- has anyone tried thisinsurance does not cover it. Below is the formulary or list of prescription drugs available to enrollees for every 2019 Medicare Advantage Plan in Wyoming and 2019 Medicare Part-D in Wyoming plans that offers additions coverage for Trelegy Ellipta 100.
As an FDA-approved treatment for COPD Trelegy is used as a once-a-day inhalant that can help open airways and lower inflammation in the lungs which can lead to improved lung function and oxygen saturation. In the Typical co-pay stage your deductible has been satisfied and Medicare pays the majority of your drug costs. Does Medicare cover Trelegy Ellipta.
Please check the formulary for different brand and generic drug names. Rinse your mouth with water without swallowing after using TRELEGY to help. Check our savings tips for co-pay cards assistance programs and other ways to reduce your cost.
If you do not have prescription drug insurance or if your medicine is not covered by your insurance talk to a pharmacist where you purchase your medicine to better understand your cost. Incruse Ellipta is covered by most Medicare and insurance plans. GoodRx has partnered with InsideRx and GlaxoSmithKline to reduce the price for this prescription.
Compare beta agonist corticosteroid combinations. Youll receive the latest information about TRELEGY sent right to your inbox or mailbox. Call your healthcare provider or get medical care right away if your breathing problems get worse if you need your rescue inhaler more often than usual or it does not work as well to relieve your symptoms.
Fungal infection in your mouth or throat thrush. COPD360social posts are monitored by Vice President of Patient Experience and COPD360social Community Manager Bill Clark as well as staff Respiratory Therapists. Check our savings tips for co-pay cards assistance programs and other ways to reduce your cost.
In 2016 the Donut Hole begins once youve spent 3310 in one year. This TRELEGY savings coupon may not be used by government beneficiaries including those eligible for or enrolled in Medicare. Check our savings tips for co-pay cards assistance programs and other ways to reduce your cost.
Trelegy Ellipta is covered by most Medicare and insurance plans. Formularies vary between drug plans and differ in the breadth of drugs covered. Check our savings tips for co-pay cards assistance programs and other ways to reduce your cost.
80 of Medicare Advantage plans and Medicare Part D plans cover Trelegy Ellipta. GoodRx has partnered with InsideRx and GlaxoSmithKline to reduce the price for this prescription. Fraudulent online pharmacies may claim to have a Trelegy generic but the medication is illegal and could be harmful if taken or used.
Original Medicare Coverage Part A and Part B does not provide coverage. Is there a Trelegy Ellipta generic available. The chart includes the plans premium and deductible for every plan that offers additions coverage for Trelegy Ellipta.
Trelegy Ellipta is covered by most Medicare and insurance plans. There are currently no generic alternatives to Trelegy Ellipta. Knowing every plans details will help you get the best coverage.
There is no generic version of Trelegy Ellipta on the market currently. Most Medicare Advantage beneficiaries 88 percent are enrolled in MA-PDs. You can also see if each plan requires Prior Authorization Step Therapy or has Drug Quantity limit for Trelegy Ellipta.
Trelegy Ellipta is covered by most Medicare and insurance plans. TRELEGY can cause serious side effects including. Medicare Advantage plans that offer prescription drug coverage are called Medicare Advantage Prescription Drug Plans MA-PD.
And vilanterol a long-acting beta2-adrenergic agonist LABA indicated for the maintenance treatment of patients with chronic obstructive pulmonary disease COPD including chronic bronchitis andor emphysema. Coverage for prescription medications like Trelegy can change depending on how a Medicare recipient chooses to receive their benefits. A formulary is a list of prescription medications that are covered if you choose to enroll with that plan.
Criteria for Approval. In the Donut Hole also called the Coverage Gap stage youll pay more for your prescriptions. For coupon eligibility purposes Medicare-eligible patients include all those age 65 and older.
There are currently no generic alternatives to Trelegy Ellipta. Every Medicare Advantage and Medicare Part-D plan will vary on covereage co-pays cost and premiums. Ug1 in Elkhart county Indiana.
Trelegy Ellipta is a combination of fluticasone furoate an inhaled corticosteroid ICS. GoodRx has partnered with InsideRx and GlaxoSmithKline to reduce the price for this prescription.