If you have prescription drug coverage through Blue Cross and Blue Shield of Texas BCBSTX this information can help you and your doctor get the most from your prescription drug coverage. By presidential executive order you can.
 Formulary Drug Lists Blue Cross Blue Shield Of Vermont
Formulary Drug Lists Blue Cross Blue Shield Of Vermont
Members under age 21 and pregnant women do not have copays.

Blue cross blue shield pharmacy card. The Mail Service Prescription Drug Benefit Program is a standard part of the Blue Cross and Blue Shield prescription drug program. As individuals in the United States are being diagnosed with COVID-19 Coronavirus we recognize BlueCross BlueShield of Western New York members may have concerns. As a current member you can access your benefits and services from your local Blue Cross Blue Shield company.
You do not need to meet any deductibles. If you are a BCBSTX member log in to Blue Access for Members SM BAM SM to check your drug list and learn more about your prescription drug benefits. Apply for individual or family medical dental and life insurance plans.
Be sure to review your benefit materials for details. If you have any questions about your prescription. While the situation is fluid and information is being updated daily one thing that will remain constant is our commitment to connecting our members to the care they need.
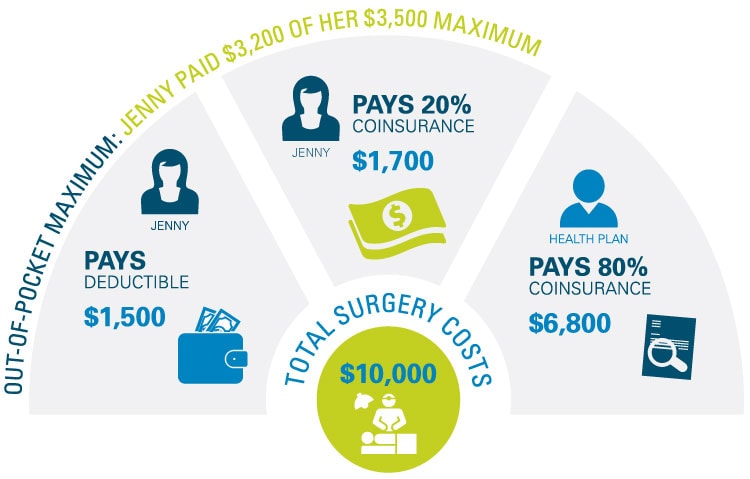
All of our members can access a network of over 60000 Preferred pharmacies across the US. Sophias BCBSTX health plan has a 3500 in-network deductible and 6000 in-network out of pocket maximum. Be sure to review your benefit materials for details.
Take your prescription bottlebag to your new pharmacy or. View a sample BCBS member card. Michigan Health Insurance Plans BCBSM.
If you are a BCBSIL member log in to Blue Access for Members SM BAM SM to check your drug list and learn more about your prescription drug benefits. If you have any questions about your prescription. To get started please have the prescribing physicians contact information and your Blue Cross Blue Shield of Massachusetts member ID card available.
You are a HealthSelect of Texas participant whose primary care provider on file with Blue Cross and Blue Shield of Texas has changed. First always be sure to have your Blue Cross Blue Shield Member ID card with you when you go to pick up your prescription. Blue Cross Blue Shield of Massachusetts BCBSMA.
To fill a prescription at one of our Preferred retail pharmacies simply show your member ID card when submitting your prescription. Enroll in a plan between now and Aug. There is no deductibleyou only pay your applicable cost share amounts based on the drug tier and your coverage type.
Enter the first three letters of the Identification Number from your member ID card. You only pay your applicable cost share amounts based on the drug tier and your coverage type. Call your new pharmacy and ask them to contact your current pharmacy or.
Ask your doctor to contact your new pharmacy. This is her in-network pharmacy cost negotiated by Blue Cross and Blue Shield so she pays a lower out of pocket amount. Administers your pharmacy benefits on behalf of Blue Cross Blue Shield of Massachusetts.
CVS Pharmacy You also can download the OTC Network app and scan products in stores to determine eligibility and check your card balance. Yes simply register with the BCBSMA MyBlue Member App to download your digital ID card or provide the information below to any network retail pharmacy. Blue Shield of California welcomes you.
Ask your doctor to send any new prescriptions to your new network pharmacy. Pharmacy management program requirements apply to specialty medications included in the NPF. If you have prescription drug coverage through Blue Cross and Blue Shield of Illinois BCBSIL this information can help you and your doctor get the most from your prescription drug coverage.
You can also get OTC medicines with a prescription from your doctor. You will receive a separate ID card for pharmacy benefits from your prescription drug benefits plan administrator. Please make sure the specialty pharmacy that you select carries the medication you need as not all medications are available at all of the specialty pharmacies listed.
Use this ID card when you pay for prescriptions at the pharmacy. Your copay is 050 for OTC medicines. Your copay for prescriptions is 3 for brand-name drugs and 1 for generic drugs.
Medications are conveniently delivered to their home and members are able to take advantage of the discount arrangement with the mail service. Where to Fill Specialty Pharmacy Medications Plans with the Blue Cross Blue Shield of Massachusetts formulary or NPF require members to fill. As a member Sophia will pay 181 for her inhaler medication for a 30-day supply.
Use the debit card at the following national retail stores. The benefit is available to members with our prescription drug card program as well as those with BlueSCRIPT the electronic claim service. Health insurance can help cover some of the costs associated with prescription medications and the pharmacist will need your insurance information to determine how much you pay and how much is covered by insurance.
Be sure to bring your member ID card with you if its your first visit to the. Then call one of the specialty pharmacies listed below to order your. Simply show your member ID card at the pharmacy.