NIA Magellan will manage non-emergent outpatient IPM services along with inpatient and outpatient cervical and lumbar spine surgeries. Select Request Member Care from the left-hand menu or contact us at the number on the members benefit card.
RadMD is available 247 except when maintenance is performed every third Thursday of the month from 9pm - midnight PST.
Nia magellan prior authorization phone number. To ensure our health plan members and providers are supported during this national state of emergency we have taken measures to support appeals being processed with no delay. NIA Magellan PTOT Fax Number. We hope you find this a helpful tool in working with NIA to provide quality care to members.
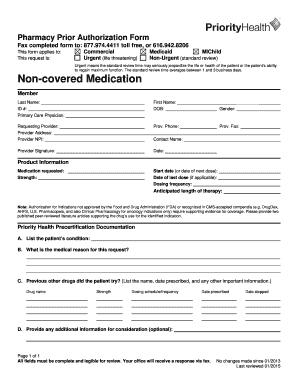
You have instant access to the imaging authorization and supporting information you need on this Web site. You may obtain prior authorization by calling 1-800-424-5657. This program is consistent with industry-wide efforts to ensure clinically appropriate quality of care.
How does the ordering provider obtain a prior authorization from NIA for an outpatient advanced imaging service. You will be able to upload requested records on the NIA website or through the NIA fax number 1-800-784-6864. What does the NIA Magellan authorization number look like.
The program includes management of non-emergent high-tech outpatient radiology services through prior authorization. MHS has contracted with National Imaging Associates Inc. Available at the point of care in electronic health records DecisionPoint improves efficiencies and reduces the time to treatment leading to increased provider and patient satisfaction.
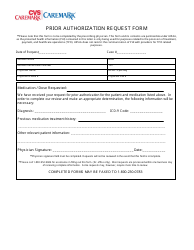
For Magellan Rx Pharmacy specialty medication needs please call us at 866-554-2673 Monday through Friday 8am 10pm Eastern. You may provide the Prescription Drug Prior Authorization form to the member and direct the member to contact their prescribing doctor to complete the form and fax it to Magellan Rx Management at 800-424-3260. If you currently mail appeals to PO Box 1495 and PO Box 2273 Maryland Heights MO we ask that instead of mailing the appeals please submit them via fax to 888-656-0701.
The doctor may need to contact Magellan Rx. Call center hours of operation are Monday through Friday 8am to 8 pm EST. Logging into NIA Magellans Website or calling NIA Magellans Call Center Information is required Name and office phone number of ordering physician Member name and ID number Requested examination Name of provider office or facility where the service will be performed Anticipated date of service.
If you have any questions about coverage and whether pre-authorization is necessary for the service you are providing contact us at the number. Medical necessity reviews are based on clinical guidelines which are available on the NIA website. The following authorization tools are available after you log in.
800-784-6864 For each authorization is it expected that we would have to upload more clinical documentation after. We welcome your feedback on how we can make our handbook even better and more helpful to you. NIA an affiliate of Magellan Health Services for radiology benefit management.
Whether submitting imaging exam requests or checking the status of ordered exams you will find RadMD to be an efficient easy-to-navigate resource. Receive an NIA Magellan tracking number not the same as an authorization number if the providers authorization request is not approved at the time of initial contact. For Assistance or Technical Support.
Providers can use either number to track the status of their request online or through an Interactive Voice Response IVR telephone system. About NIA NIA has provided industry-leading specialty healthcare management services to improve health. In some cases the ordering provider may instead receive an NIA Magellan tracking number not the same as an authorization number if the providers authorization request is not approved at the time.
Not included in this program and do not require prior authorization through NIA. Our team is available 24 hours including weekends and holidays for urgent requests. For Prior Authorizations please call the phone number on the back of the member ID card.
The NIA Magellan authorization number consists of 8 or 9 alpha-numeric characters. Prior authorization is a time-consuming process for health plans providers and patients. Comments may be e-mailed to NIA.
Effective management of costly and complex conditions Magellans. If this is an urgent prescription have the member call Magellan Customer Service at 877-879-9922.