If you see an out-of-network provider you need to submit the claim yourself. Monday through Friday from April 1 through September 30 or send us an.
 Provider Directory Blue Advantage Administrators Of Arkansas
Provider Directory Blue Advantage Administrators Of Arkansas
If you select the Alternative Option you must submit relevant data or records showing a higher contribution percentage.
Blue cross blue shield medicaid arkansas. In Eastern Wisconsin Anthem Blue Cross and Blue Shield is the trade name of Compcare Health Services Insurance Corporation for its insurance policies offered through the BadgerCare Plus program an independent licensee of the Blue Cross and Blue Shield. Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. If you use a network doctor or hospital your claims will be submitted by that provider.
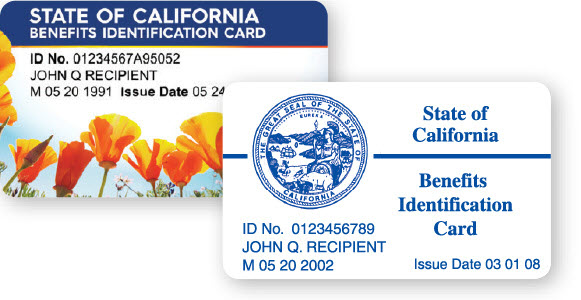
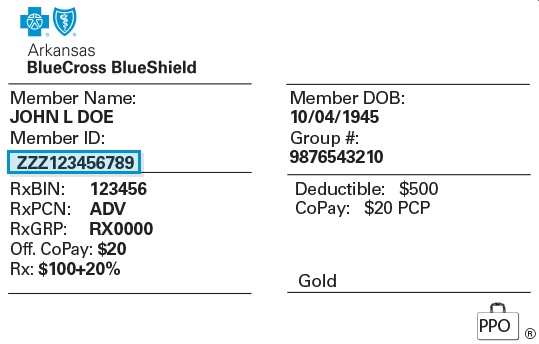
Arkansas Blue Cross and its affiliates have more than 2500 employees. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield. View a sample BCBS member card.
The purpose of a Coverage Policy is to inform members and their physicians why certain medical procedures may or may not be covered under Arkansas Blue Cross and Blue Shield health plans. Executive Director Arkansas Advanced Care a Medicaid subsidiary Arkansas Blue Cross Blue Shield Jan 2017 - Dec 2018 2 years. Arkansas Blue Cross Blue Shield AR BCBS submissions and ERA retrieval is now only available via the Availity Clearinghouse as of December 31 2020.
Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. Arkansas Blue Medicare offers HMO PFFS PPO and PDP plans with Medicare contracts. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield.
Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. If you are NOT currently enrolled in an Arkansas Blue Cross and Blue Shield plan and would like to talk to someone about a Medi-Pak Supplement plan call 1-844-298-2442 8 am. As a current member you can access your benefits and services from your local Blue Cross Blue Shield company.
Arkansas Blue Medicare Plus is the trade name for Arkansas Blue Medicare PPO plans. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield. Please click this link to access the instructions for enrolling with Availity.
Arkansas Blue Medicare is an affiliate of Arkansas Blue Cross and Blue Shield. Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield.
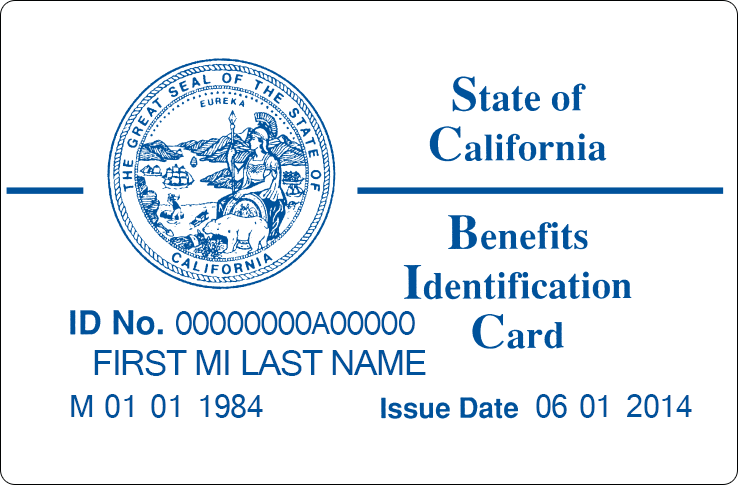
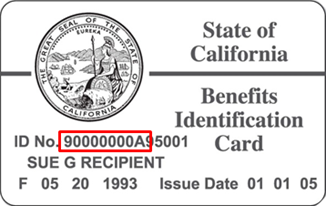
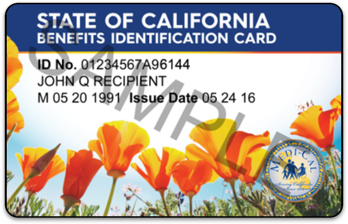
Enrollment in Arkansas Blue Medicare depends on contract renewal. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield. Enter the first three letters of the Identification Number from your member ID card.
The Blue Cross and Blue Shield Association is comprised of 36 independent locally operated Blue Cross and Blue Shield Plans that collectively provide health care. Copyright 2001-2021 Arkansas Blue Cross and Blue Shield. The medical director of Arkansas Blue Cross and Blue Shield has established specific coverage policies addressing certain medical procedures or technologies.
8 pm 7 days a week from October 1 through March 31 or 8 am. Instructions for submitting your claim are on the claim form available here. In addition to these specific Coverage Policies all Arkansas Blue Cross and Blue Shield.
The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. Founded in 1948 Arkansas Blue Cross and Blue Shield an independent licensee of the Blue Cross and Blue Shield Association is the largest health insurer in Arkansas. Otherwise the Default Option will be used.
You must submit a completed claim form or alternative documentation via fax or mailing address. Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. Little Rock Arkansas Area.
Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. If you have any questions please call us at 602-439-2525. Blue Cross Blue Shield.
How to File a Claim with Blue Cross Blue Shield and Ambetter Insurance. Arkansas Blue Cross and Blue Shield is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. Blue Cross Blue Shield Settlement co JND Legal Administration PO Box 91390 Seattle WA 98111.