But again as long as your plan isnt grandmothered or grandfathered your total out-of-pocket charges cant exceed 8150 in 2020 as long as you stay in-network and follow your insurers rules for things like referrals and prior authorization. Lets say your health insurance plans allowed amount for an office visit is 100 and your coinsurance is 20.
 Coinsurance After Deductible How To Choose Between 100 And 0
Coinsurance After Deductible How To Choose Between 100 And 0
You typically pay coinsurance after meeting your annual deductible.
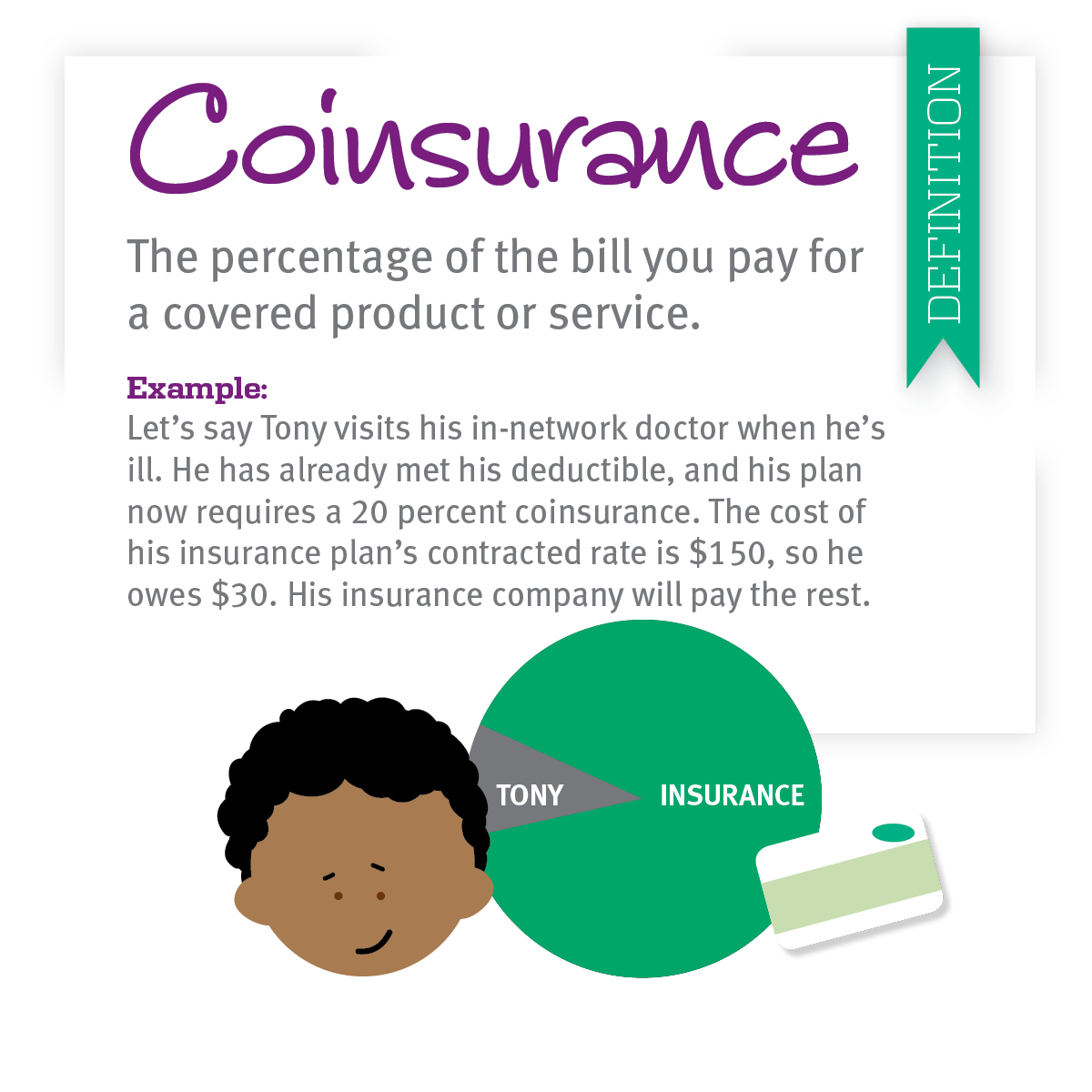
What does it mean 30 coinsurance after deductible. If youve paid your deductible. Coinsurance is the amount you will pay for a medical cost your health insurance covers after your deductible has been met. Coinsuranceis what youthe patientpay as your share toward a claim.
When can coinsurance and deductibles be waived. The 30 percent you pay is your coinsurance. Coinsurance is often 10 30 or 20 percent.
Coinsurance is often 10 30 or 20 percent. When you look at your policy youll see your coinsurance shown as a fractionsomething like 8020 or 7030. 4 but she would also need to foot a bigger portion of the whole bill by 10000 in services but she would also need to foot a bigger portion of the whole bill by 10.
For example if your coinsurance is 20 percent you pay 20 percent of the cost of your covered medical bills. After you pay the 4000 deductible your health plan covers 70 of the costs and you pay the other 30. Coinsurance is an additional cost that some health care plans require policy holders to pay after the deductible is met.
An example of paying coinsurance and your deductible would be if you have 1000 in medical expenses and the deductible is 100 with 30 percent coinsurance. It is your share of the medical costs which get paid after you have paid the deductible for your plan. Your deductible if you werent aware is the amount you have to pay.
Out-of-pocket maximum of 5000. There are plans that offer 100 after deductible which is essentially 0 coinsurance. An example is Affordable Care Act ACA plans.
You must pay 4000 toward your covered medical costs before your health plan begins to cover costs. Before reaching your deductible you have to pay all of your medical costs. Coinsurance is a way of saying that you and your insurance carrier each pay a share of eligible costs that add up to 100 percent.
When you pay coinsurance you split a certain cost with the insurance company at a ratio determined by the terms of your insurance plan. Coinsurance is a form of cost-sharing or splitting the cost of a service or medication between the insurance company and consumer. You pay 20 of 100 or 20.
The 30 percent you pay is your coinsurance. The percentage of costs of a covered health care service you pay 20 for example after youve paid your deductible. However coinsurance only applies after you spend enough to reach your deductible.
What does this mean 0 coinsurance after deductible. Its usually a percentage of the approved medical expense. Coinsurance is an additional cost that some health care plans require policy holders to pay after the deductible is met.
You start paying coinsurance after youve paid your plans deductible. Once youve met your deductible you might pay 20 of the cost of the health service or procedure for instance. Coinsurance is your portion of costs for health care services after youve met your deductible.
The insurance company pays the rest. What does 40 coinsurance after deductible mean. For example your plan pays 70 percent.
For instance if you have a 10000 surgery bill your 30 coinsurance will be a whopping 3000. Now if your office visit costs 200 and you have 30 coinsurance you will pay 60 of the bill in addition to your copay. Coinsurance is the share of the cost of a covered health care service that you pay after youve reached your deductible.
This makes coinsurance riskier for you since it is more difficult to set a budget for. Copays often apply regardless of whether youve reached your deductible. Youve paid 1500 in health care expenses and met your deductible.
Out-of-pocket maximum of 5 Your health plan has a. The bill from the ER is 2000 but if you had gone to your in-network primary care physician and then received a referral for the X-rays at an in-network provider. And then received a referral for the X-rays at an in-network provider000 deductible.
When you pay coinsurance you split a certain cost with the insurance company at a ratio determined by the terms of your insurance plan. This means that once your deductible is reached your provider will pay for 100 of your medical costs without requiring any coinsurance payment. Once you reach the deductible your health insurance plan will pick up a percentage of the health care costs and youll pay for the rest.
Your insurance company would pay the balance. The phrase 40 Coinsurance after deductible means that you may be responsible for 40 of the approved part of the bill plus the delta between what they bill and what they cover. Lets use 20 coinsurance as an example.
Coinsurance is a portion of the medical cost you pay after your deductible has been met. As mentioned earlier coinsurance is the percentage of health care services youre responsible for paying after youve hit your deductible for the year. When you go to the doctor instead of paying all costs you and your plan share the cost.
For example if you have a 20000 surgery bill your 30 coinsurance will be a whopping 6000.






:max_bytes(150000):strip_icc()/Humana-37822291d42b426e88d39955991c59c1.png)