Medications not on the list are considered non-formulary. Has your doctor prescribed a drug thats not on.
A formulary is a list of covered drugs selected by our plan in consultation with a team of health care providers which represents the prescription therapies believed to be a necessary part of a quality treatment program.

What does formulary mean. In addition to being present in the medication or supply search results the formulary status is also indicated below the medication. The formulary often is structured in tiers or classes of medications. The list contains information about how the drugs are made and why they are used.
A formulary is a continually updated list of prescription drugs approved for reimbursement by the PBMs payer client. Not only are they against the spirit and the letter of Anglican formularies they are against one of the decrees of the Council of Nicaea as we point out. A formulary is a list of generic and brand name prescription drugs covered by your health plan.
A book listing pharmaceutical substances and formulas for making medicinal. Its their way of providing a wide range of effective medications at the lowest possible cost. A drug formulary refers to the list of drugs that a particular health insurance plan will cover.
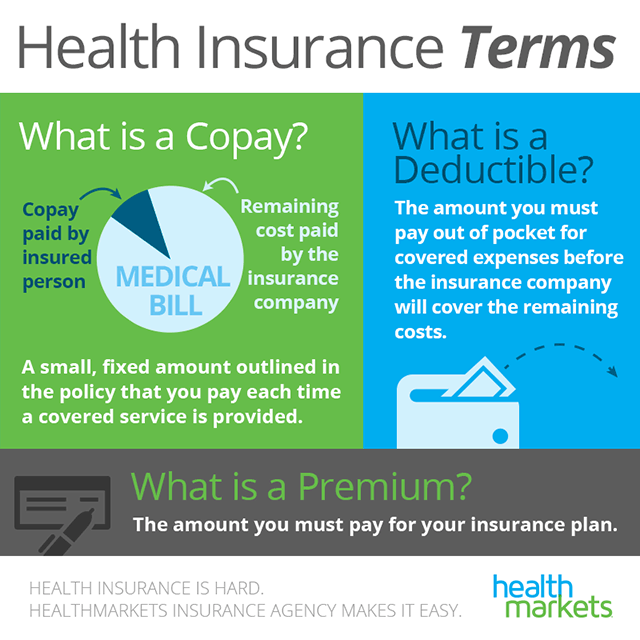
Formulary Originally a collection of formulas used in the preparation of medicines but now used for a book of drug actions side effects and dosage for the use of prescribing doctors. You may be asked to pay a copay of 5 10 20 or more depending on the drug. A formulary is a list of covered drugs.
Insurance Coverage for Non-formulary Drugs. Each plan determines which specific drugs it will include on its formulary. Each Medicare Part D prescription drug plan and Medicare Advantage plan Part C that includes drug coverage has a formulary.
Medical Definition of formulary. Among the most important tools used by PBMs to manage specialty drug costs are drug formularies. What does this mean.
Our plan will generally cover the drugs listed in our formulary as long as the drug is medically. Usually prescription drugs in the formulary are grouped into separate tiers or benefit categories according to drug costs. A book containing a list of medicinal substances and formulas see national formulary.
What does a drug formulary cover. In drchrono medications and supplies are labeled with formulary symbols indicated by one or two letters and a color code. A collection or system of formulas.
Formulary pharmacopeia adj pharmacology a book containing a compilation of pharmaceutical products with their formulas and methods of preparation postexposure prophylaxis is an integral part of the pharmacopeia in preventing severe disease after acute infections. Health insurance providers use a formulary to classify prescription medications for which they provide coverage. PBMs typically develop a basic formulary and offer it to payers who may customize it.
An official list of generic and brand name pharmaceutical drugs. Noun formularies 1 A collection of set forms especially for use in religious ceremonies. Stand-alone Medicare Part D Prescription Drug Plans and Medicare Advantage plans with prescription drug coverage all have lists of covered prescription drugs called formularies.
Medicare Part D plans can change formulary or drug list designs each year and with the new plan year your Medicare prescription drug plan may have implemented utilization management or drug usage ma. A set form of words. A formulary is a list of drugs or supplies that indicate the greatest overall value after evaluation for both safety and effectiveness.
A formulary is a listing of brand name and generic medications that are preferred by your insurance company. The insurer can change the list at its discretion. Your health plan may only help you pay for the drugs listed on its formulary.
Drug formularies convey what medications will be covered and at what level using a tiered approach in which the higher the tier the greater the.