Select HMO Plan for CalPERS Coverage for. Covered Medical Benefits Cost if you use an In-Network Provider Cost if you use a Non-Network Provider Overall Deductible.
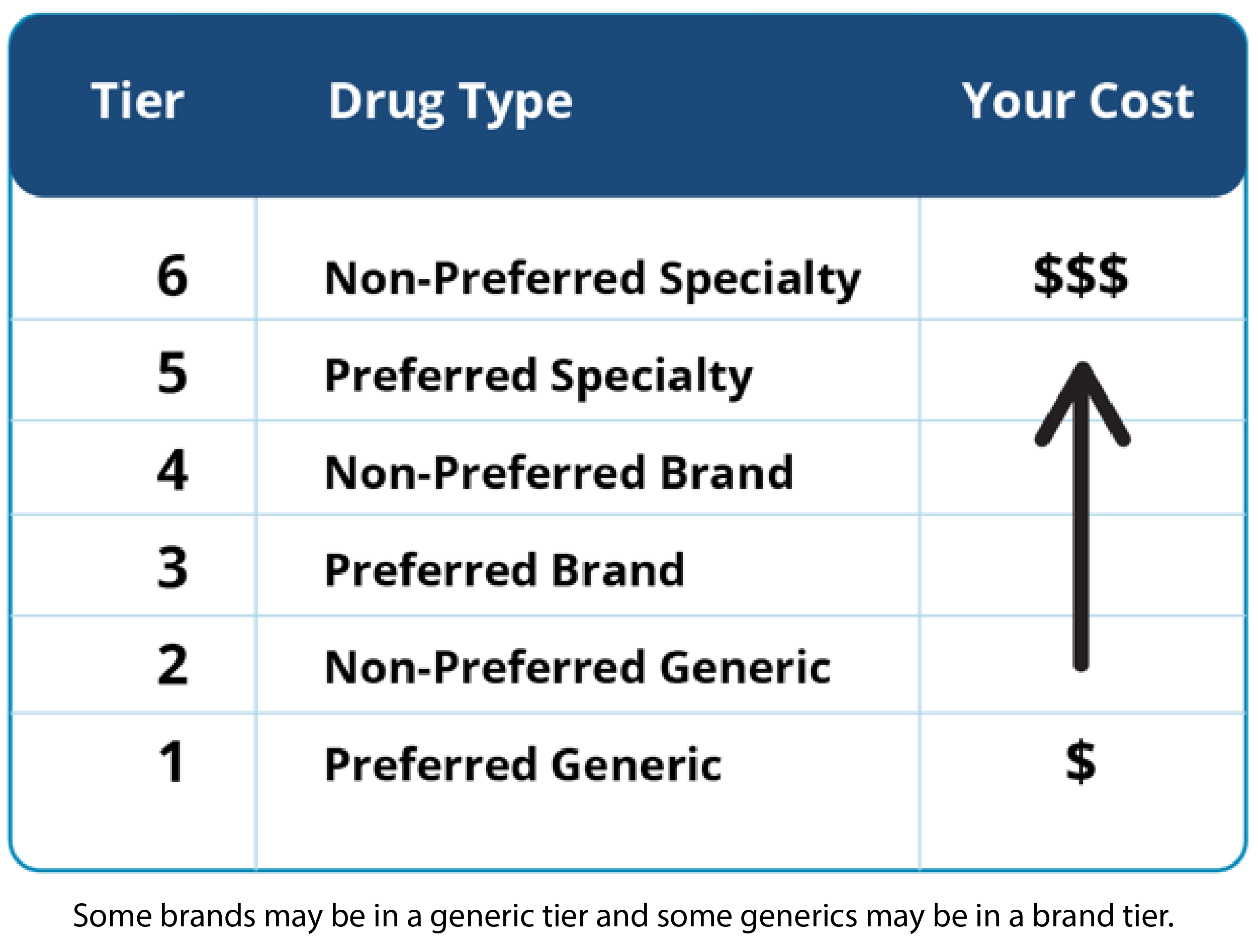
Note that you can select just one tier and any number of health insurance plans within that tier.
Anthem blue cross select hmo coverage. And is it worth your money at all. This booklet tells you all about your health care plan and its benefits. If you need care after normal business hours your Doctor may have several options for you.
After Hours Care. Anthem Blue Cross. With Anthem Blue Cross Select HMO Anthem provides you both narrow and full network tiers.
This summary does not reflect each and every benefit exclusion and limitation which may apply to the coverage. Individual Family Plan Type. HMO The Summary of Benefits and Coverage SBC document will help you choose a health plan.
It tells you about what kinds of care this plan covers and doesnt cover. Anthem Blue Cross HMO benefits are covered only when services are provided or coordinated by the primary care physician and authorized by the participating medical group or independent practice association IPA. Anthem Blue Cross Select HMO Coverage Period.
The Summary of Benefits and Coverage SBC document will help you choose a health. Tell them you are an Anthem Blue Cross Select HMO Member Have your Member Identification Card handy. What this Plan Covers What it CostsCoverage forIndividual Spouse Family Plan TypeHMO Questions.
You should call your. Tell them the reason for your visit. The Summary of Benefits and Coverage SBC document will help you choose a health.
Anthem MediBlue Prime Select HMO has a monthly drug premium of 0 and a 0 drug deductible. About Anthem Blue Cross. Anthem Blue Cross Select Basic Plan.
Modified Premier HMO 15100 Custom RX 10204040 Your Network. This plan Anthem MediBlue Select HMO is offered by Anthem Blue Cross. Anthem MediBlue Select HMO H0544-058 is a 2021 Medicare Advantage Plan or Medicare Part-C plan by Anthem Blue Cross available to residents in California.
Except OBGYN services received within the members. Anthem Blue Cross Select HMO is here to serve you. Along with Kaiser Anthem Blue Cross offers the most popular HMOs in California.
Welcome to Anthem Blue Cross Select HMO Thank you for choosing our health plan. 0 person Not covered. Anthem Blue Cross.
01012019 12312019. We would like to show you a description here but the site wont allow us. The SBC shows you how you and the plan would share the cost for covered health care services.
Also keep in mind that PPO plans offer you national. Health Maintenance Organization HMO Evidence of Coverage and Disclosure Form for the Basic Plan Effective January 1 2018. This covers the basic prescription benefit only and does not cover enhanced drug benefits such as medical benefits or hospital benefits.
Anthem Blue Cross. When it says plan or our plan it means Anthem MediBlue Select HMO Anthem Blue Cross is an HMO plan with a Medicare contract. The SBC shows you how you and the plan would share the cost for covered health care services.
Except OB GYN services received within the members medical group IPA and services for mental and nervous disorders and substance abuse. Anthem Blue Cross Your Plan. 1500 single 3000 family Not covered.
2018 Anthem Blue Cross Select HMO Plan. Anthem Blue Cross 21555 Oxnard Street Woodland Hills California 91367 Phone Number. City of Los Angeles Narrow Network HMO Select 15100 Coverage for.
One great option for those looking for low copays and solid coverage is the Anthem Blue Cross Select HMO. This Anthem Blue Cross and Blue Shield plan offers a 0 Part D Basic Premium that is not below the regional benchmark. This plan reportedly combines low monthly premiums with lots of coverage but what exactly is covered under this HMO.
Anthem Blue Cross HMO benefits are covered only when services are provided or coordinated by the primary care physician and authorized by the participating medical group or independent practice association IPA. You can select from a variety of plan types including HMO PPO EPO and Health Savings Account-compatible plans. The SBC shows you how you and the plan.
Individual Family Plan Type. Combined Evidence of Coverage and Disclosure Form. When this Evidence of Coverage says we us or our it means Anthem Blue Cross.
Select HMO Your Network. The Anthem MediBlue Select HMO has a monthly premium of 0 and has an in-network Maximum Out-of-Pocket limit of 900. The Doctors office may ask you for your group or Member ID number.
Individual Family Plan Type. 01012014 12312014 Summary of Benefits and Coverage. It tells you what you have to do or what has to happen so you.
Select HMO Plan for CalPERS Coverage for. Anthem Blue Cross offers the health insurance coverage and choices you and your employees want and need. This plan includes additional Medicare prescription drug Part-D coverage.
This summary of benefits is a brief outline of coverage designed to help you with the selection process.

/medi-weightloss-program-4157710-a-bc198a45b7d340ca81476c48071f9eff.jpg)



.png)
