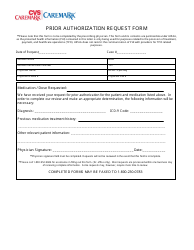
For inquiries or questions related to the patients eligibility drug copay or medication delivery. The CVS Caremark Prior Authorization Request Form can be used to request coverage for a non-formulary medication or one which is more expensive than those which are typically covered by the insurance company.
 Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.

Cvs caremark specialty pharmacy prior authorization form. Prior Authorization can ensure proper patient selection dosage drug administration and duration of. CVS Caremark administers the prescription benefit plan for. CVS Caremark administers the prescription benefit plan for the patient identified.
CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs. CVS Caremark is dedicated to helping physicians manage and help their patients who are suffering from complex disorders and require specialized therapies and personalized care. CVSCaremark Prior Rx Authorization Form.
This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment. We are CVS Specialty.
You can refill prescriptions monitor order status make payments and much more anytime online. Select the appropriate CVS Caremark form to get started. Formulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name.
To make an appropriate determination providing the most accurate diagnosis for the use of the prescribed medication is necessary. CoverMyMeds automates the prior authorization PA process making it the fastest and easiest way to review complete and track PA requests. Signing above I hereby authorize CVS Specialty Pharmacy andor its affiliate pharmacies to complete and submit prior authorization PA requests to payors for the prescribed medication for this patient and to attach this Enrollment Form to the PA request as my signature.
Please contact the Specialty Customer Care Team. These are just some of the ways we can help you manage your specialty condition. Please respond below and fax this form to CVS Caremark toll-free at 1-866-249-6155.
And well be here when you need us because you are our specialty. Case Review Unit CVS Caremark Specialty Programs Fax. Please respond below and fax this form to CVS Caremark toll-free at 1-866-249-6155.
CoverMyMeds is CVS Caremark Prior Authorization Formss Preferred Method for Receiving ePA Requests. Send completed form to. If you have questions regarding the prior authorization please contact CVS Caremark at 1-866-814-5506.
Prior Authorization Request. CVS Caremark Specialty Pharmacy 2211 Sanders Road NBT-6 Northbrook IL 60062 Phone. Start Saving on Select Meds When You Transfer Your Prescriptions over to Publix Pharmacy.
For even more convenience use our digital tools to manage your medication. The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. Specialty Pharmacy Services Information and Forms.
For all other questions regarding the submission of your request please contact CVS Caremark. Anzeige From Savings to Sync Your Refills Reminders Publix Pharmacy Is at Your Service. Start Saving on Select Meds When You Transfer Your Prescriptions over to Publix Pharmacy.
Brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. Select your specialty therapy then download and complete the appropriate enrollment form when you send us your prescription. Prior Authorization Request.
We offer access to specialty medications and infusion therapies centralized intake and benefits verification and prior authorization assistance. CVS Caremark Specialty Pharmacy 2211 Sanders Road NBT-6 Northbrook IL 60062 Phone. CVS Caremark does not perform the prior authorization review but will forward any clinical.
Anzeige From Savings to Sync Your Refills Reminders Publix Pharmacy Is at Your Service. For FEP drugs requiring online prior authorization. The below form must be completed in its entirety by the medical practitioner prescribing the drug.
Select the Provider tab Tools Resources then Forms. Authorize CVS Specialty Pharmacy andor its affiliate pharmacies to complete and submit prior authorization PA requests to payors for the prescribed medication for this patient and to attach this Enrollment Form to the PA request as my signature.






